otitis externa
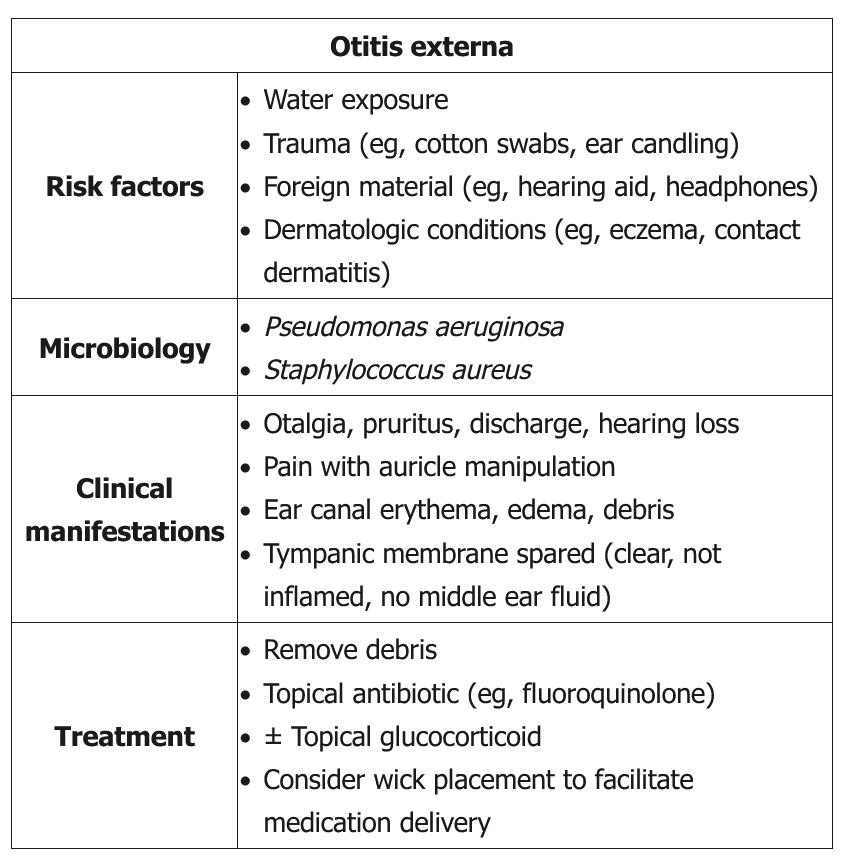
This patient has acute otitis externa (OE), likely from swimming. The most common organisms causing OE are Pseudomonas and Staphylococcus species. Initial treatment includes thoroughly cleaning the ear canal to remove cerumen and other debris and nonsteroidal anti-inflammatory drugs for pain control. An otoscope can directly visualize the canal, and a wire loop can gently remove debris and cerumen. Irrigating the ear canal with a 1:1 dilution of 3% hydrogen peroxide is also effective in patients with intact tympanic membranes.
Mild OE (pruritus with minimal canal edema) usually improves with combined acidifying agent (eg, acetic acid) to inhibit bacterial growth in the ear canal and topical glucocorticoids to decrease inflammation. Moderate (pain, pruritus, partial canal occlusion) to severe (intense pain, canal occlusion, fever) OE requires combined topical antibiotics (eg, quinolones, polymyxin B, neomycin), antiseptics, and glucocorticoids with possible wick placement. Both ofloxacin and ciprofloxacin have excellent coverage against P aeruginosa and S aureus.
Oral antibiotics do not significantly improve uncomplicated OE but are added in immunocompromised patients and for deep-tissue infections beyond the ear canal. These patients are also at risk for malignant OE, with the infection spreading to the skull base, and usually need otolaryngology referral. This patient with moderate OE may first be treated with a topical antibiotic and glucocorticoid (Choices B and C). If she does not improve within 3 days, she requires culture of the ear canal or referral to an otolaryngologist (Choices A and D).
Malignant
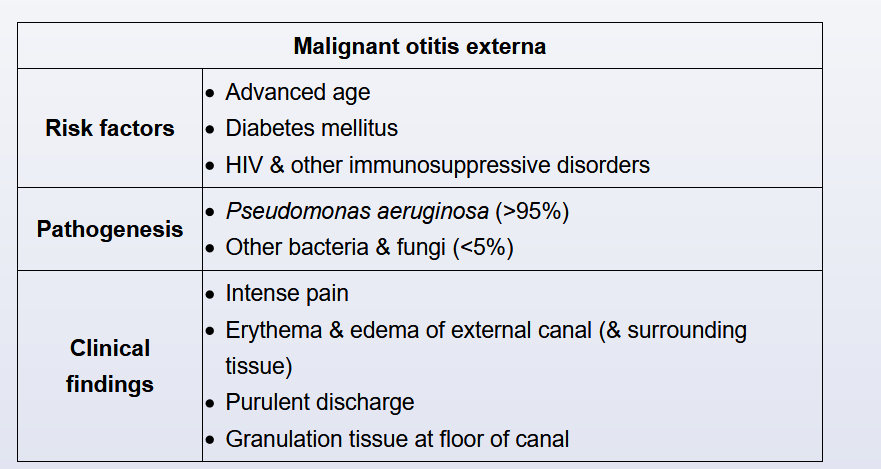
This patient has an acutely inflamed ear canal with purulent drainage and granulation tissue formation. In an older patient with comorbid diabetes (or other immunosuppressing conditions) this is concerning for malignant otitis externa (MOE). MOE usually begins as a superficial external otitis but progresses rapidly to involve the adjacent bones at the base of the skull. A recent history of aural irrigation (ie, for cerumen disimpaction) is a common finding.
Patients with MOE have marked pain with manipulation of the ear. Systemic signs (eg, fever) are common. Granulation tissue in the external canal at the bone-cartilage margin is pathognomonic for MOE but is not always present. There may be severe edema and occlusion of the canal, but the tympanic membrane is usually intact. Most (>95%) cases of MOE are due to Pseudomonas aeruginosa, although other bacteria and fungi (eg, Aspergillus) are occasionally seen. Untreated MOE can progress rapidly to involve the skull base, temporomandibular joint, and cranial nerves, leading to osteomyelitis and cranial nerve palsies.
Pseudomonas aeruginosa is responsible for almost all cases of malignant otitis externa (MOE), and systemic anti-pseudomonal therapy is required. Fluoroquinolones (eg, ciprofloxacin) are the preferred initial treatment, but anti-pseudomonal penicillins (eg, piperacillin), with or without aminoglycosides, and third-generation cephalosporins (eg, ceftazidime) are also effective and can be used for patients with contraindications to quinolones or suspected antimicrobial resistance.
Treatment is usually initiated with intravenous medication. Inflammatory markers (eg, erythrocyte sedimentation rate, C-reactive protein) correlate with disease activity, and the patient can be converted to oral therapy when these tests normalize. 6-8 weeks of therapy is recommended.